Timisoara_Med 2021, 2021(2), 1; doi:10.35995/tmj20210201
Case Report
Assessment of Valvular Oxidative Stress in a Young Patient with Primary Severe Mitral Regurgitation
1
Department of Functional Sciences – Pathophysiology, “Victor Babeș” University of Medicine and Pharmacy, 2 EftimieMurgu Sq., 300041 Timișoara, Romania; ionica.loredana@umft.ro (L.N.I.); daninamuntean@umft.ro (D.M.M.); sturza.adrian@umft.ro (A.S.)
2
Center for Translational Research and Systems Medicine, “Victor Babeș” University of Medicine and Pharmacy, 2 EftimieMurgu Sq., 300041 Timișoara, Romania
3
Department of Cardiology – Cardiology II, “Victor Babeș” University of Medicine and Pharmacy, 2 EftimieMurgu Sq., 300041 Timișoara, Romania; alex.pescariu@yahoo.com (A.S.P.); mornoscristi@yahoo.com (C.M.); adina_ionac@rdstm.ro (A.I.)
4
Center for Cardiovascular Diseases Research, Institute of Cardiovascular Diseases, 13A Gheorghe Adam Str., 300310 Timișoara, Romania
5
Department of Cardiology – Cardiovascular Surgery, “Victor Babeș” University of Medicine and Pharmacy, Institute of Cardiovascular Diseases, 13A Gheorghe Adam Str., 300310 Timișoara, Romania; horea.feier@umft.ro
*
Correspondence: sosdean.raluca@umft.ro (R.Ș.); ctluca@cardiologie.ro (C.T.L.)
How to cite: Ionică, L.N.; Șoșdean, R.; Pescariu, A.S.; Mornoș, C.; Muntean, D.M.; Ionac, A.; Sturza, A.; Luca, C.T.; Feier, H. Assessment of Valvular Oxidative Stress in a Young Patient With Primary Mitral Regurgitation. Timisoara Med. 2021, 2021(2), 1; doi:10.35995/tmj20210201.
Received: 15 May 2021 / Accepted: 20 August 2021 / Published: 29 December 2021
Abstract
:Mitral valve regurgitation (MR) is the most common valvular heart disease. Diagnosing and managing mitral regurgitation is often challenging and requires a structured approach, integrating findings on history, physical examination and imaging. A common cardiac anomaly is myxomatous mitral valve prolapse. Excess myxomatous leaflet tissue, bileaflet prolapse or billowing, chordae elongation and annular dilatation are all features of Barlow’s disease. Currently, there is no successful pharmacological treatment available to prevent or slow its progression. Here, we report the case of a 30-year-old male patient, with no previous significant medical background and no medication at home, who was diagnosed with severe mitral regurgitation at a regular check-up and was admitted to our clinic with mild exertion dyspnea and fatigue. Transthoracic echocardiography showed intensely thickened mitral leaflets with a myxomatous appearance, prolapse of the middle scallop of the posterior leaflet (P2), apparently with ruptured chordae, and severe mitral regurgitation with a holosystolic eccentric jet. While oxidative stress is a central pathomechanism of cardiovascular disease, information regarding valvular oxidative stress in the literature is rather scarce. In this respect, we assessed oxidative stress through confocal microscopy in a sample of a mitral valve harvested during valvular surgery. We found an increased production of reactive oxygen species in the mitral valve sample that was alleviated after incubation with the angiotensin 2 receptor type I (AT1) antagonist irbesartan. This case is worth mentioning as a starting point for a prospective study aimed at assessing the role of valvular oxidative stress and mitochondrial dysfunction in patients with various degrees of primary and secondary mitral regurgitation.
Keywords:
primary severe mitral regurgitation; Barlow’s disease; transesophageal echocardiography; oxidative stress; angiotensin 2 receptor antagonistIntroduction
Mitral regurgitation is the most common valvular disorder worldwide that usually requires surgical intervention, affecting over two million people, with an alarming increase in the prevalence with advanced age [1]. Mitral regurgitation may occur as a result of mitral valve leaflet disease and/or defects in the mitral valve apparatus, or as a consequence of left ventricular dysfunction [2]. This condition may be classified as either primary or secondary. Primary regurgitation, also known as degenerative or organic regurgitation, is caused by an intrinsic lesion of the mitral valve apparatus. Secondary mitral regurgitation, frequently called functional or ischemic, is a disease of the left ventricle [3].
Degenerative mitral valve disease, most often mitral leaflet prolapse and/or flail, is the most common cause of primary mitral regurgitation, with two major phenotypes: fibroelastic deficiency and Barlow’s disease [4].
Younger patients with a persistent murmur are more likely to have Barlow’s disease, a condition distinguished by an abundance of leaflet tissue. The chordae and leaflets appear thickened, redundant and elongated [5]. During systole, multiple scallops of either anterior and posterior leaflets prolapse or flail into the left atrium [6]. Prolapse is estimated to occur in approximately 2.4% of the general population using existing echocardiographic diagnostic criteria. Just 5–10% of patients with mitral valve prolapse have severe regurgitation. Most of the time, mitral valve prolapse is associated with chronic mitral regurgitation, but complications (i.e., chordae rupture, infective endocarditis) can lead to the onset of acute mitral regurgitation. The rate at which regurgitation progresses is an interindividual variable. Factors that influence progression are primarily anatomical and related to the etiology of the lesion, with patients with mitral valve flail and mitral ring dilation experiencing faster progression.
Despite the fact that Barlow’s disease was first described in the early 1960s, no significant risk factors have been identified, and the mechanisms underlying mitral valve prolapse are still partially understood. Moreover, although Barlow’s disease is the most common cause of non-ischemic mitral regurgitation in developed countries, currently, there is no successful pharmacological treatment available to prevent or slow its progression. Studies in humans aimed at examining the cellular and molecular mechanisms underlying the different stages of myxomatous degeneration development and progression are rather scarce. One potential contributor is the local, persistent oxidative stress [1].
Here, we present the case of a young patient with primary severe mitral regurgitation that underwent surgical intervention, describing the molecular mechanisms underlying the treatment and his evolution.
Case Report
A 30-year-old male patient, with no previous significant medical background and no medication at home, was diagnosed with severe mitral regurgitation at a regular check-up, about three weeks prior to presentation at our clinic. He presented with mild exertion dyspnea and fatigue and was admitted to the hospital for further investigations and treatment. Clinical examination revealed regular heart sounds and a late systolic murmur with a mid-to-late systolic click.
The patient’s blood pressure at arrival was 120/70 mmHg. The ECG at admission showed a sinus rhythm, HR = 70 bpm, and standard blood tests were within normal limits.
Transthoracic echocardiography showed intensely thickened mitral leaflets with a myxomatous appearance, prolapse of the middle scallop of the posterior leaflet (P2), apparently with ruptured chordae, severe mitral regurgitation with a holosystolic eccentric jet (reaching the anterior wall of the left atrium) and left atrial enlargement. Left ventricular systolic function was within normal limits, with a left ventricular ejection fraction (LVEF) of 55%, left ventricular end-diastolic volume (LVEDV) of 150 mL and left ventricular end-systolic volume (LVESV) of 75 mL. There was also ultrasound evidence of mild tricuspid regurgitation and mild secondary pulmonary hypertension, with a normal systolic function and normal right ventricle size.
The transesophageal echocardiography with 3D reconstruction revealed a suggestive aspect for Barlow’s disease (Figure 1): P2 scallop flail with chordal rupture (surgical view), and in the color Doppler section (Figure 2), we visualized severe mitral regurgitation with an eccentric jet adjacent to the anterior mitral valve.
The next step was to initiate treatment with a loop diuretic carefully administered to relieve the pulmonary pressures.
Given the presence of heart failure symptoms, minimally invasive mitral valve repair was performed, with triangular P2 resection and ring annuloplasty. Postoperatively, the patient’s evolution was favorable, without complications. He was discharged after 7 days, with a significantly improved clinical status.
Identification of pathways leading to the development of diffuse myxomatous degeneration of leaflet tissue is of major clinical relevance, given the fact that myxomatous mitral valve disease affects young adult patients. Therefore, our purpose was to investigate valvular oxidative stress using a sample of a mitral valve harvested during valvular surgery, but after first receiving the patient’s permission in a signed consent document.
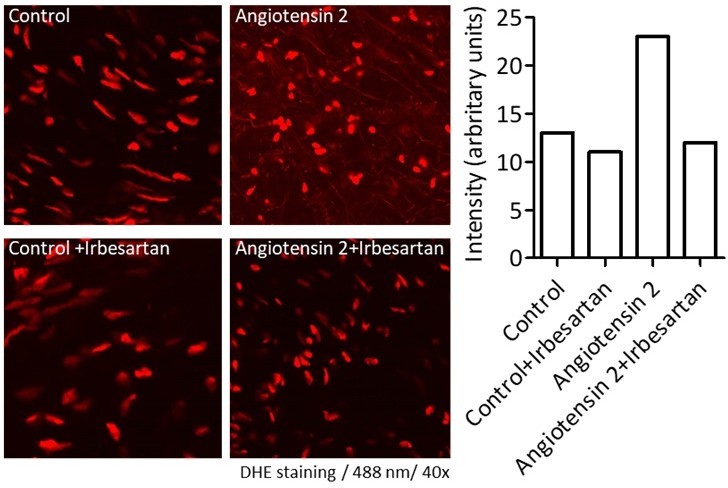
We assessed reactive oxygen species (ROS) production after sample incubation with angiotensin 2 (100 nM, 12 h) with and without the angiotensin 2 receptor type 1 (AT1) antagonist (irbesartan 10 microM, 12 h), by confocal microscopy using the dihydroethidium (DHE) marker. Our choice was irbesartan, a strong and selective antagonist of AT1 receptors that is often used to treat mild to moderate hypertension. Previous research has shown that irbesartan possesses anti-inflammatory properties at the endothelium level by inhibiting TNF alpha and IL6, as well as a strong antioxidant effect on many body tissues. Briefly, the valve sample was frozen, cut in cryosections (20 μm thick) and incubated with DHE for 30 min. The slides were mounted and analyzed using a confocal microscope (Olympus Fluoview FV1000). Images were obtained using laser excitation at 488 nm and emission at 610 nm. Image analysis was performed using ImageJ software.
We observed that the level of ROS in the mitral valve sample prelevated from our patient was alleviated after incubation with the angiotensin 2 receptor type I (AT1) antagonist (irbesartan 10 microM), especially after angiotensin 2 incubation (Figure 3).
Discussion
Prolapse of the myxomatous mitral valve is a typical cardiac abnormality. Barlow’s disease is characterized by an abundance of myxomatous leaflet tissue, prolapse or billowing of bileaflet tissue, chordae elongation and annular dilatation with or without calcification [2].
Besides echocardiography, up to now, there are no reliable biomarkers available for the identification of this pathology. Early therapies aimed to reduce leaflet stress in genetically susceptible individuals may theoretically delay the progression of myxomatous mitral valve degeneration and prevent late valvular complications such as severe mitral valve regurgitation, arrhythmia or infective endocarditis.
Following a routine check-up, the patient was diagnosed with mitral valve prolapse without significant regurgitation, being asymptomatic at the time. He developed symptoms of heart failure after the onset of a complication: chordae rupture, which culminated in severe mitral regurgitation as a secondary complication.
Interestingly, there is one in vitro study that used surgically excised mitral leaflet specimens and reported (poster presentation) that myxomatous mitral valve changes might be pharmacologically modifiable by an angiotensin receptor 2 blocker [3].
Since the patient lacked anyrenin–angiotensin–aldosterone system medication, we thought to incubate ex vivo the mitral valve sample with angiotensin 2 (12 h, 100 nM). This led to increased ROS production that was mitigated by the incubation with the angiotensin 2 receptor type 1 (AT1) antagonist irbesartan (10 microM). These findings add new information about the role of the renin–angiotensin system in the control of the oxidative stress response in our patient’s case, highlighting the protective effect of the AT1 receptor antagonist irbesartan. Certainly, a number of questions remain unsolved, and further study will be needed to understand the pathomechanisms underlying this phenomenon.
Deroyer et al. performed a study aimed at characterizing novel biomarkers of mitral regurgitation in order to better understand the underlying pathomechanisms and allow the diagnosis and monitoring of the disease [4]. Modulation of various blood proteins’ expression was examined in patients suffering from different grades of mitral regurgitation (mild, moderate and severe) vs. healthy controls. To this end, several routine clinical assays and the multi-analyte profile technology targeting 184 proteins were used. High-density lipoprotein, apolipoprotein-A1, haptoglobin and haptoglobin-α2 chain levels significantly decreased proportionally to the degree of mitral regurgitation as compared to the controls. High-density lipoprotein and apolipoprotein-A1 levels were associated with an effective regurgitant orifice area and regurgitant volume.
Apolipoprotein-A1 was an independent predictor of severe mitral regurgitation. Moreover, myxomatous mitral valves were studied by immunocytochemistry, and the authors observed an increase in LC3, the marker of autophagy, in myxomatous mitral valves compared with healthy mitral valves.
Hagler et al. tested the hypothesis that increased transforming growth factor-β (TGF-β) signaling and ROS are major contributors to pro-fibrotic gene expression in human mitral valves. Studies were performed on 48 samples of human mitral valve tissue collected during surgery at the Mayo Clinic, Rochester (24 controls were non-myxomatous mitral valves explanted from cardiac transplant recipients, and 24 samples were collected from individuals with myxomatous mitral valve degeneration during mitral valve repair procedures). Using qRT–PCR, the authors found that increased expression of TGF-β1 in mitral valves from humans with myxomatous degeneration was associated with increased expression of connective tissue growth factor (CTGF). They concluded that activation of TGF-βsignaling is a major contributor to fibrosis and matrix remodeling in myxomatous mitral valve degeneration and is amplified by increased oxidative stress. Treatments aimed at reducing TGF-β activation and mitigating oxidative stress in early myxomatous mitral valve degeneration may slow its progression [5].
Gladden et al. identified increased xanthine oxidase as a source of oxidative stress, as well as clusters of small mitochondria as a hallmark of a bioenergetic defect, in the left ventricle of patients with isolated mitral regurgitation and an LVEF of >60% [1].
More recently, in 43 patients, Sogia et al. investigated the osteoprotegerin levels, a molecule that has been associated with cardiometabolic disorders and increased cardiovascular mortality and also linked to oxidative stress, in patients who underwent mitral valve repair due to mitral valve prolapse [6]. They assessed the levels of oxidized and reduced glutathione by means of liquid chromatography-tandem mass spectrometry. They reported increased oxidative stress and osteoprotegerin concentrations in patients with mitral valve prolapse as compared to the controls.
Conclusions
This case is worth mentioning as a starting point for a prospective study aimed at assessing the role of valvular oxidative stress and mitochondrial dysfunction in patients with various degrees of primary and secondary mitral regurgitation. Here, we firstly reported an increase in local oxidative stress in the presence of angiotensin 2 in a mitral valve harvested from a young patient with primary severe mitral regurgitation. This effect was mitigated after treating the sample with an angiotensin 2 receptor type 1 (AT1) antagonist. The sources and types of ROS will be further investigated in the presence vs. absence of other cardiovascular drugs as well.
Author Contributions
Conceptualization, L.N.I., R.Ș., H.F.; writing—original draft preparation, L.N.I., R.Ș., A.S.; writing—review and editing, R.Ș., C.M., D.M.M., A.I., A.S., C.T.L.; supervision, A.S.P., D.M.M., A.I., H.F.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Gladden, J.D.; Ahmed, M.I.; Litovsky, S.H.; Darley-Usmar, V.; McGiffin, D.C.; Lloyd, S.G.; Gupta, H.; Dellʼitalia, L.J.; Schiros, C.G.; Denney, T.S. Oxidative Stress and Myocardial Remodeling in Chronic Mitral Regurgitation. Am. J. Med. Sci. 2011, 342, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Barlow, J.B.; Pocock, W.A. Billowing, floppy, prolapsed or flail mitral valves? Am. J. Cardiol. 1985, 55, 501–502. [Google Scholar] [CrossRef]
- Malev, E.; Kim, G.; Vasina, L.; Omelchenko, M.; Zemtsovsky, E. P100Angiotensin II receptor blockers in modulation of transforming growth factor-b cardiac effects in mitral valve prolapse. Cardiovasc. Res. 2014, 103, S17. [Google Scholar] [CrossRef]
- Deroyer, C.; Magne, J.; Moonen, M.; Le Goff, C.; Dupont, L.; Hulin, A.; Radermecker, M.; Colige, A.; Cavalier, E.; Kolh, P.; et al. New biomarkers for primary mitral regurgitation. Clin. Proteom. 2015, 12, 25. [Google Scholar] [CrossRef] [PubMed]
- Hagler, M.A.; Hadley, T.M.; Zhang, H.; Mehra, K.; Roos, C.M.; Schaff, H.V.; Suri, R.M.; Miller, J.D. TGF-β signalling and reactive oxygen species drive fibrosis and matrix remodelling in myxomatous mitral valves. Cardiovasc. Res. 2013, 99, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Songia, P.; Porro, B.; Chiesa, M.; Myasoedova, V.; Alamanni, F.; Tremoli, E.; Poggio, P. Identification of patients affected by mitral valve prolapse with severe regurgitation: A multivariable regression model. Oxid. Med. Cell. Longev. 2017, 2017, 6838921. [Google Scholar] [PubMed]
Figure 1.
Transesophageal echocardiography with 3D reconstruction (surgical view): thickened mitral leaflets, and P2 scallop flail with chordal rupture.
Figure 1.
Transesophageal echocardiography with 3D reconstruction (surgical view): thickened mitral leaflets, and P2 scallop flail with chordal rupture.
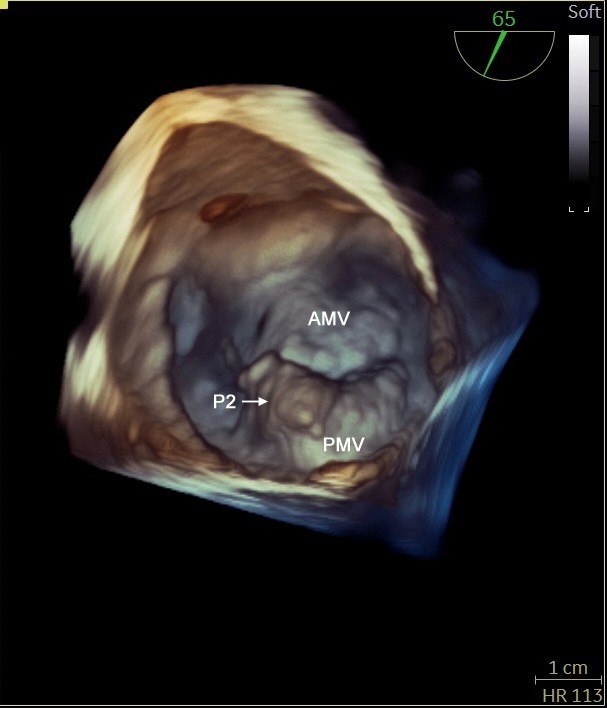
Figure 2.
Two-dimensional color Doppler section: severe mitral regurgitation with an eccentric jet adjacent to the anterior mitral valve.
Figure 2.
Two-dimensional color Doppler section: severe mitral regurgitation with an eccentric jet adjacent to the anterior mitral valve.
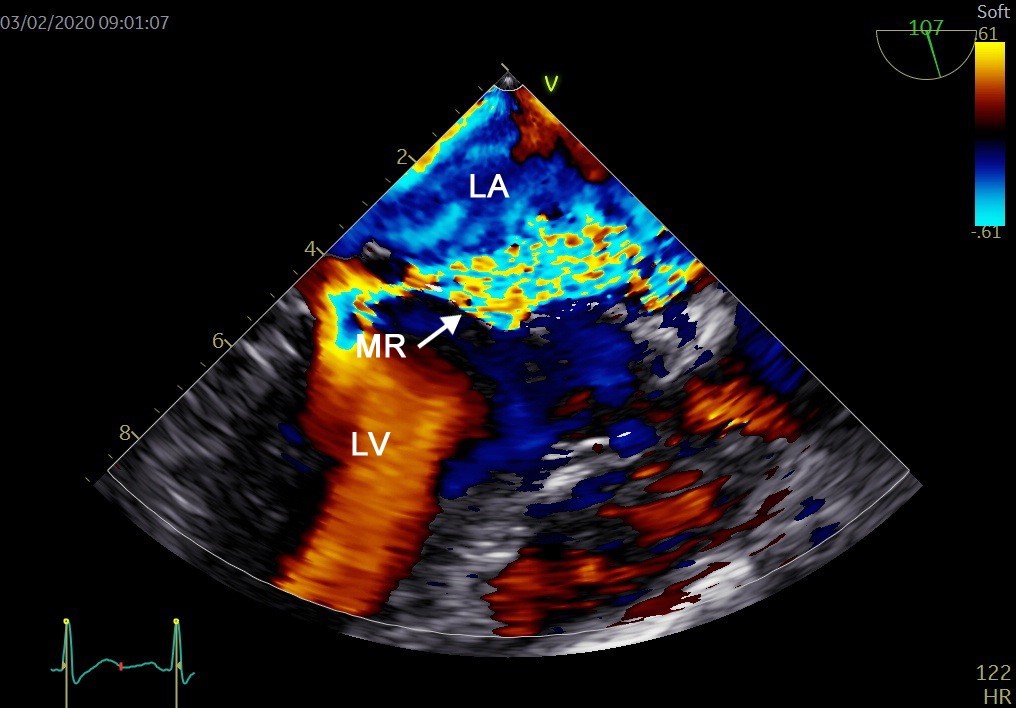
Figure 3.
DHE staining of the mitral valve after incubation with angiotensin 2 (100 nM) with and without irbesartan (10 µM, 12 h).
Figure 3.
DHE staining of the mitral valve after incubation with angiotensin 2 (100 nM) with and without irbesartan (10 µM, 12 h).
© 2021 Copyright by the authors Licensed as an open access article using a CC BY 4.0 license

