Timisoara_Med 2022, 2022(1), 4; doi:10.35995/tmj20220104
Case Report
Acute Ulcerative Gingivitis with Pseudomembranous Tonsillitis: A Case Report of Vincent’s Stomatitis in an Immunocompetent Patient
1
A.J. Institute of Dental Sciences, Mangalore 5750041, India; rksdental@gmail.com
2
Yenepoya Dental College, Yenepoya University, Mangalore 575018, India
*
Correspondence: roopashri.r.k@gmail.com; Tel.: +91-9448910793
How to cite: Kashyap, R.R.; Kashyap, R.S. Acute Ulcerative Gingivitis with Pseudomembranous Tonsillitis: A Case Report of Vincent’s Stomatitis in an Immunocompetent Patient. Timisoara Med. 2022, 2022(1), 4; doi:10.35995/tmj20220104.
Received: 31 August 2021 / Accepted: 12 April 2022 / Published: 7 May 2022
Abstract
:Acute necrotizing ulcerative gingivitis or Vincent’s stomatitis is a painful infectious condition of gingiva due to endogenous bacteria. It is an uncommon disease of gingiva, usually seen in patients with impaired immunity, which may be due to some underlying systemic diseases such as HIV infection, malignancy, or diabetes mellitus. Rarely, it is also seen in immunocompetent patients living a stressful life. Here, we report a case of Vincent’s stomatitis with the acute ulcerative involvement of gingiva and pseudomembranous ulceration of tonsils in a general medical practitioner living a busy life.
Keywords:
gingivitis; psychological stress; stomatitis; tonsillitisIntroduction
Acute necrotizing ulcerative gingivitis (ANUG) is a rapidly destructive, non-communicable, opportunistic infection caused by endogenous anaerobic microorganisms which is a relatively forgotten disease entity in this era [1,2]. In developing countries such as India, people have a hectic lifestyle, trying to meet the needs and demands of their family and society. This unknowingly results in increased stress in life. We report a case of Vincent’s infection in a medical practitioner due to a stressful lifestyle.
Case Report
A 40-year-old female patient presented with soreness in the gums and teeth, of two days duration. History revealed that the patient had noticed soreness and bleeding from the gums only while brushing for a week. For the last two days the patient had increased soreness in the gums throughout the day, which was aggravated while eating food. She had felt that her back teeth were slightly elevated. She had associated soreness in the tonsils and a fever of 102° F for a day. The patient had consumed Augmentin 625 mg twice daily and paracetamol 500 mg for fever. The patient felt no relief after taking the medicines and had observed an increase in the severity of lesions. She also complained of a metallic taste, halitosis and increased salivation. The patient was a medical practitioner on a vegetarian diet and had a hectic lifestyle sleeping an average of six hours per day.
Examination revealed mild fever 100.6° F and 3–4 tender, bilateral submandibular lymph nodes. The intraoral examination revealed halitosis and generalized erythematous tender and enlarged marginal gingiva, more predominant at the mandibular left molar region. Marginal gingiva in the mandibular molar region showed ulcerations and interdental gingiva was enlarged beyond the occlusal surface, creating a pseudo-pocket, measuring about 6mm in length (Figure 1). All the posterior teeth were tender on percussion.
A yellowish white pseudomembrane was seen covering both the inflamed tonsils (Figure 2). Small ulcers were noted at the tonsil, palate and lower gingival level.
Clinical features of pseudomembranous tonsillitis and acute gingivitis with halitosis were suggestive of anaerobic infection, more likely due to a fuso-spirochetal infection. Upon removing the pseudomembrane from the tonsil, small ulcerations measuring about 2 mm in diameter were noticed. Routine hemogram showed a lower hemoglobin level at 10 gm/dL and an abnormal high platelet count at 558,000/mm3. The patient was tested negative for HIV and hepatitis B. The intraoral periapical radiograph in relation to the lower left molar showed widening of periodontal space at the periapex. The patient was prescribed Metronidazole 400 mg thrice daily together with Augmentin 625 mg twice daily for seven days, paracetamol 500 mg for fever s.o.s, warm saline irrigation, povidone–iodine gargle thrice daily and chlorhexidine mouthwash 3–4 times per day. After 1 week, symptoms had subsided, but enlarged interdental and marginal gingiva in relation to the lower left second molar were still evident. The culture and sensitivity of the swab specimen showed no isolation of pathogens. As the patient was feeling generalized weakness, she was supplemented with a multivitamin tablet for a month. After 20 days the gingiva had returned to normal size and patient was feeling completely recovered (Figure 3).
Discussion
Vincent’s stomatitis is an endogenous polymicrobial infection mainly affecting patients with impaired immunity. Plaut and Vincent are pioneers who independently, in the 1890's, recognized the fusiform-spirochete association with this disease [3,4]. Most of the time, the term acute necrotizing ulcerative gingivitis (ANUG) is used to describe the acute ulcerative disease affecting the gingiva, and Vincent’s angina is the term used for fuso-spirochetal infection of the oropharynx and throat, with a painful membranous ulceration of the throat [5]. In our patient, tonsils as well as the gingiva were affected, which is a rare occurrence.
The predominant anaerobic organisms currently implicated in ANUG are Fusobacterium necrophorum, Prevotella intermedia, Fusobacterium nucleatum, Porphyromonas gingivalis, as well as Treponema and Selenomonas spps [2]. Many predisposing factors have been proposed for the pathogenesis of ANUG, such as poor oral hygiene, smoking, emotional stress, nutritional deficiency, systemic diseases or an altered immune system [5]. However, after ruling out all the other causes and understanding the hectic routine due to the heavy work schedule, we concluded that stress was the main underlying factor resulting in ANUG in our patient.
The diagnostic triad for ANUG is pain, gingival ulceration, and bleeding. The secondary clinical signs of ANUG include: halitosis, pseudomembranes, a “wooden” sensation to the teeth, metallic taste, tooth mobility, ropy saliva, lymphadenopathy, fever, and malaise [6]. Though the clinical features vary from patient to patient, some of the most common features were also seen in our patient. However, the pseudomembrane was covering only the tonsils and not any part of gingiva. Probably, as our patient was immunocompetent, the features of ANUG were not as severe as mentioned in previous studies [5,7]. The cultures of samples are often negative—because of their fastidiousness, these organisms are difficult to isolate [8]. Culture and sensitivity of the pseudomembrane swab taken from the tonsil of our patient was also negative for isolation of pathogens.
The management should focus on removal of microbial accumulation and local factors. Hence, we aimed at the non-surgical management of the condition. Based on the microbial nature, antibiotics such as penicillin and metronidazole are the drugs of choice. Systemic antibiotics, however, do not eliminate local etiological factors. Antibacterial mouthwashes such as 0.12% chlorhexidine are helpful in controlling the infection locally [1,5]. Usually, surgical debridement and recontouring are recommended after the acute phase has been resolved. However, as our patient was immunocompetent, we opted to wait for recovery before any sort of intervention. Within 20 days the gingiva had returned to normal, avoiding the need for surgical management.
Conclusions
ANUG is a rare disease in immunocompetent individuals. Stressful routines in the developing countries may act as a main predisposing factor, as is evident in this case. This is one of the first cases to report the incidence of ANUG in a financially competent educated patient. This report highlights the need for enough repose for the doctor community who themselves may fall prey to such diseases if personal care is neglected.
Author Contributions
Conceptualization, R.R.K. and R.S.K.; methodology, R.S.K.; software, not applicable.; validation, R.R.K. and R.S.K.; formal analysis, R.R.K. and R.S.K.; investigation, R.R.K. and R.S.K.; resources, R.R.K. and R.S.K.; data curation, R.R.K. and R.S.K.; writing—original draft preparation, R.R.K.; writing—review and editing, R.R.K. and R.S.K.; visualization, R.R.K. and R.S.K.; supervision, R.S.K.; project administration, R.R.K. and R.S.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Murayama, Y.; Kurihara, H.; Nagai, A.; Dompkowski, D.; Van Dyke, T.E. Acute necrotizing ulcerative gingivitis: Risk factors involving host defense mechanisms. Periodontology 2000 1994, 6, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Folayan, M.O. The epidemiology, etiology, and pathophysiology of acute necrotizing ulcerative gingivitis associated with malnutrition. J. Contemp. Dent. Pract. 2004, 5, 28–41. [Google Scholar] [CrossRef] [PubMed]
- Johnson, B.D.; Engel, D. Acute necrotizing ulcerative gingivitis: A review of diagnosis, etiology, and treatment. J. Periodontol. 1986, 57, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; Kent, P.; Lennon, J.M.; Logan, L.K. Acute necrotising ulcerative gingivitis in an immunocompromised young adult. BMJ Case Rep. 2015, 2015, bcr2015211092. [Google Scholar] [CrossRef] [PubMed]
- Newman, M.G.; Takei, H.; Klokkevold, P.R.; Carranza, F.A. Carranza's Clinical Periodontology, 11th ed.; Elsevier Health Sciences: Chatswood, Australia, 14 February 2011. [Google Scholar]
- Horning, G.M.; Cohen, M.E. Necrotizing ulcerative gingivitis, periodontitis, and stomatitis: Clinical staging and predisposing factors. J. Periodontol. 1995, 66, 990–998. [Google Scholar] [CrossRef] [PubMed]
- Malek, R.; Gharibi, A.; Khlil, N.; Kissa, J. Necrotizing ulcerative gingivitis. Contemp. Clin. Dent. 2017, 8, 496. [Google Scholar] [CrossRef] [PubMed]
- Brook, I. Spectrum and treatment of anaerobic infections. J. Infect. Chemother. 2016, 22, 1–3. [Google Scholar] [CrossRef] [PubMed]
Figure 1.
Marginal gingival proliferation with ulceration in relation to the mandibular left second molar.
Figure 1.
Marginal gingival proliferation with ulceration in relation to the mandibular left second molar.

Figure 2.
Pseudomembrane formation and ulceration in both the tonsils.
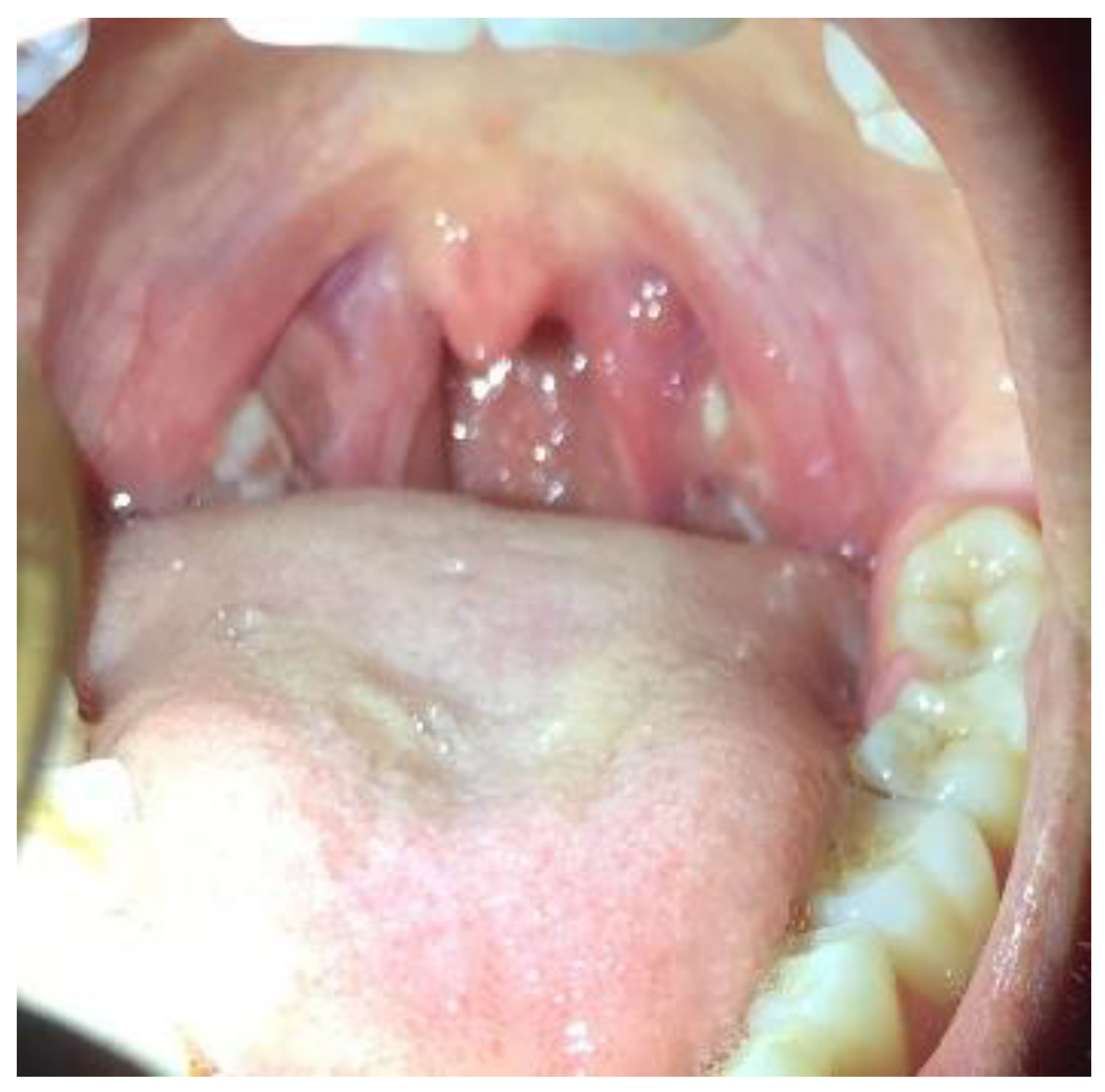
Figure 3.
Healed gingiva after 20 days.

© 2022 Copyright by the authors. Licensed as an open access article using a CC BY 4.0 license.
