Timisoara_Med 2023, 2023(1), 3; doi:10.35995/tmj20230103
Article
Investigating the Connection between Parental Education and Children’s Oral Health: An Extensive Examination in Western Romania for 11–14-Year-Olds
1
Translational and Experimental Clinical Research Centre in Oral Health, Department of Preventive, Community Dentistry and Oral Health, University of Medicine and Pharmacy “Victor Babes”, 300040 Timisoara, Romania; dumitrescu.ramona@umft.ro (R.D.); jumanca.daniela@umft.ro (D.J.); daninnegru@gmail.com (D.N.); balean.octavia@umft.ro (O.B.); pascaioanagiorgiana@gmail.ro (I.G.P.); roancea@umft.ro (R.O.); galuscan.atena@umft.ro (A.G.)
*
Correspondence: savarosianu@yahoo.com; Tel.: +40740315848
How to cite: Dumitrescu, R.; Sava-Rosianu, R.; Jumanca, D.; Negru, D.; Bălean, O.; Pașca, I.G.; Oancea, R.; Gălușcan, A. Investigating the Connection between Parental Education and Children’s Oral Health: An Extensive Examination in Western Romania for 11–14-Year-Olds. Timisoara Med. 2023, 2023(1), 3; doi:10.35995/tmj20230103.
Received: 12 June 2023 / Accepted: 26 June 2023 / Published: 5 July 2023
Abstract
:(1) Background: This research is part of the Romanian oral health survey for children, aiming to determine correlations between the oral health status of 11–14-year-old schoolchildren and their parents’ educational levels, taking into account preventive behaviour and socioeconomic parameters. (2) Methods: a representative sample of 133 schoolchildren (72 boys and 61 girls), average age 12.26 ± 0.6 years, was examined by calibrated dentists. After obtaining ethical approval, a visual examination using ICDAS criteria was performed to classify visual caries lesion severity. Statistical analyses of the data were performed using SPSS 23, Spearman’s rank correlation and the Pearson correlation. (3) Results: Mean DMFT within the sample was 2.93 ± 2.70. High school was the most common level of education completed by the parents. A positive relationship was recorded between the mother’s level of education and the frequency of toothbrushing in children (rs = 0.02 *, p < 0.01), as well as with oral hygiene aids (rs = 0.17 *, p < 0.05). A negative significant correlation resulted between D3T index and the mother’s level of education (rs = −0.26 **, p < 0.01), as well as with the father’s education (rs = −0.17 **, p < 0.01). (4) Conclusions: The results of this study show that high caries prevalence could be associated with low educational level and socio-economic county-level variables, having an impact on the presence and severity of such lesions, as well as the absence of existing treatments.
Keywords:
schoolchildren; caries; preventive behaviour; parental education; DMFTIntroduction
The WHO’s latest statements say that although major improvements in oral health can be seen, globally the burden of disease is still high. The Global Burden Disease (GBD 2017) study states that in both temporary and permanent dentition the prevalence of dental caries is highest, and it is also second in incidence among oral diseases [1]. Dental caries still remains the most important public oral health disease, because it affects large numbers of people worldwide, mainly in developing countries. Epidemiological studies of the World Health Organization’s Oral Health Program show that the prevalence and severity of dental caries in children living in certain developed countries has declined over the past two decades, while in others it has increased [2].
Oral health as a determinant of quality of life has been widely considered to be a method of quantifying the impact of diseases and disorders on individuals and society. Quality of life is used to assess the general consequences of poor oral health in different communities of children, adults or families [3]. Health is defined by the World Health Organization not just as the absence of pathological issues, but also taking into account mental, physical and social well-being [4]. According to the definition of the International Dental Federation (FDI), oral health includes the ability to smell, chew, speak, smile, taste, swallow, touch and express different feelings through facial expression in the absence of pain, discomfort or complex craniofacial conditions. Based on the definitions [5], oral health has several dimensions in nature, being related to physical, emotional, psychological and social aspects integrated into general health and well-being. Oral health is constantly adapting and being perceived differently, allowing individuals to eat, talk, smile and socialise without feeling embarrassed, or feeling pain or discomfort. Oral cavity diseases, with their growing prevalence in many low- and middle-income countries (LMICs), are closely connected to social and economic changes, making them a significant global public problem and public health concern [1].
Being both chronic and progressive over time, tooth decay affects children from an early age. The financially and socially disadvantaged in society are disproportionately affected by diseases of the oral cavity. Socioeconomic status is strongly correlated with the prevalence and severity of oral diseases. Thus, oral health problems are sensitive markers of a poor social level and early indicators of poor general health status [6]. Oral health inequalities are directly related to social and economic determinants, representing the first signs of poor oral health in the population [7].
The WHO [8] highlighted that despite significant improvements in community oral health, oral cavity diseases are still an important global public health problem affecting general health and quality of life. Dental caries affects more than 90% of the global population, being one of the most common non-communicable diseases (NCDs). Caries prevalence, the number of caries, and caries experience show an increasing trend even in economically developed countries. Economic inequalities are strong determinants for childhood dental caries [8,9,10,11,12].
Family environments are a key factor that support healthy choices and lifestyles, coping skills and effectiveness in dealing with life. Satisfaction and trust in the dental care system reinforces the value of oral health [13]. The hypothesis that the way parents adopt brushing habits influences their children’s tooth brushing behaviour has been confirmed by international studies [14]. Thus, educational programmes addressed at children as well as parents could improve caries experience and quality of life [15].
Parents’ behaviours directly influence caries prevalence in young children, showing that oral health interventions should focus on the entire family. Parents’ behaviour has a positive impact on their children’s oral health. The higher the parents’ level education, the better their children’s oral self-care [16]. Aspects of maternal oral hygiene and habits influence children’s oral self-care, thus highlighting the importance and role of female figures for their children’s oral health status [17]. Therefore, education should develop programmes that focus on these issues [18].
Caries experience varies in children, in accordance with culture, age and general health, but also parental education [19]. The existence of temporary teeth alongside permanent teeth can be seen to start from the age of 6–7 years. At this age, caries prevalence is usually high and forming sanogenic oral health behaviours is extremely important. Therefore, parents’ good oral hygiene and knowledge related to oral health are of great importance [20]. Families with low income and a low level of education also show a low attendance at regular dental check-ups, which has a negative impact on their oral health [21].
Complications of dental caries go beyond clinical symptoms like pulpal affectation and pain, having a major impact on the children’s daily performances, development and overall quality of life, lowering their self-esteem and affecting the child’s well-being [22,23]. As demonstrated by other studies, there is a correlation between early childhood caries, poor oral health status and quality of life [24]. Complex dental care represents, on the one hand, a great financial burden, and on the other hand stress and disturbance to the wellbeing of the entire family [25].
While at an international level the concern of the scientific community is reflected in an increased availability of data on children’s oral health, in the case of Romania the number of scientific studies carried out so far is low, and data collected are limited to very small areas and usually in urban or peri-urban agglomerations. This research is part of the first Romanian Oral Health Study on the dental status of 6- and 12-year-old schoolchildren, aiming to analyse the main risk factors that have an influence on the prevalence and severity of dental caries, taking into consideration individual level variables and the objective reality in which children live [25,26,27]. Taking into account that improving oral health is part of the universal health coverage agenda by 2030, according to the WHO’s Resolution on Oral Health, the results of this research can be useful for identifying the most effective means and methods to promote oral health in the target group, Romanian schoolchildren [28].
This paper aims to analyse the prevalence of dental caries in 12-year-old children in the western part of Romania, based on several types of data obtained both from oral health assessment questionnaires and examinations, and to assess the correlation between their oral health status and the parental level of education.
Material and Methods
In 2019–2020, a cross-sectional epidemiological investigation was devised and executed, having obtained authorisation from the World Health Organization (WHO). The Ministry of Health provided assistance, and the study adhered to the regulations outlined in the General Data Protection Regulation of 2018. The study’s methodology garnered approval from various authoritative bodies, including the local school authorities, the school inspectorate at the regional level, the Romanian Ministry of Health (Opinion No. 3411/05.04.2018), the Ministry of Education (Opinion No. 1573/12.03.2019) and the University of Medicine and Pharmacy “Victor Babeș”, Timisoara, Romania (No. 29/28.09.2018).
This study was conducted on a group of 133 children, boys and girls, representing nine educational institutions located in the Western region of Romania, namely, from the regions of Banat, Central Transylvania and North-Western Transylvania (Avram Iancu Unirea Secondary School, Alba County; Secondary School Arad, Arad county; Nicolae Popoviciu Beiuș Secondary School, Bihor county; Pietroasa Secondary School, Bihor county; Banatul High School with Sports Program Timișoara, Timis county; Periam High School, Timiș county; I.C. Brătianu Hațeg, Hunedoara County; Măureni Secondary School, Caras-Severin County; Brateiu Secondary School, Sibiu County). Children attending 6th grade were included in our study. The primary criteria for inclusion in the study was an average age of 12 years. The sixth-grade classes in each school were the only ones included in the study. While the exact participation rate was not documented, it is reasonable to estimate that at least 90% of only the 6th grade children from these 9 schools were included. To ensure a randomised and stratified sample, the total number of students in each county was calculated as a percentage of the total number of children enrolled in the 8th grade National Examination across all schools in Romania. This process involved evaluating publicly available information from 4696 schools [26]. The estimation of the number of children to be included in each county was based on the percentage share. Subsequently, this number was divided according to the type of locality (urban or rural) to obtain the final target number of assessments. To select schools for the study, MS Excel’s randomisation function was utilised, ensuring the selection of one urban and one rural school for each county (refer to Figure 1). In total, nine schools were chosen, encompassing both rural and urban areas. The predictors at the school level included the Development Index (LHDI 2011), as provided by Dumitru Sandu [25]. This index is a sociological measure that combines various county-level variables, such as education stock, life expectancy at birth, average age of the adult population, available living space, number of private cars per 1000 inhabitants, and average household gas consumption. Factor analysis was employed to aggregate these variables, and the resulting scores were relevant for evaluating the county’s labour force potential and economic prospects.
Prior to conducting the study, parental or legal guardian consent was obtained to ensure informed consent for the children’s participation. The selection of schools and classrooms followed the WHO procedure for oral health status surveys, aiming to represent the area’s population despite the small sample size. Before the examination, participants’ parents or legal guardians submitted informed consent. The 12-year-olds themselves completed the questionnaire, which covered topics such as parenting education, dental visit frequency and reasons, dental care habits, and sweet consumption.
The examination was performed by examiners who underwent necessary calibration prior to data collection. The calibration process involved examining 21 subjects. The inter-examiner kappa coefficient ranged from 0.74 to 0.86, and the intra-examiner kappa coefficient ranged from 0.81 to 0.92. The kappa coefficient consistently fell within the excellent range for obturations and within the good to excellent range for lesion severity. None of the children in the sample were re-examined.
The children underwent examinations during the data collection process, which took place in a classroom or any available room. The teacher was present throughout the procedure. Special LED front lighting sources, commonly used in dentistry, along with examination kits, were utilised. Radiographs were not employed for diagnosis due to the examination environment. Inclusion criteria encompassed children without chronic diseases who were not taking medication, regardless of their gender, race, or socioeconomic status. The children needed to be cooperative to meet the inclusion criteria. On the other hand, children undergoing fixed orthodontic treatment or displaying uncooperative behaviour were excluded. Prior to the examination, each participant arrived with informed consent and a signed questionnaire provided by their parents or caregivers. The visual caries lesions were classified using the ICDAS criteria. The collected data were coded, entered into examination charts, stored electronically, and linked to the questionnaire and consent form of each participant.
Data were gathered utilising the Oral Health Questionnaire for Children, a tool developed by the World Health Organization and outlined in the 2013 Edition of WHO Oral Health Surveys-Basic Methods. To ensure accuracy, the English version of the questionnaire underwent translation by two independent translators, with any disparities resolved through a face-to-face meeting. Additionally, two experts, one holding a PhD in educational psychology and the other in developmental psychology, were consulted to assess the readability of the Romanian version of the Child Oral Health Questionnaire.
The questionnaire encompasses 15 questions that fell into two categories: preventive behaviour and dietary habits. These dimensions significantly impact oral health and dental care. Preventive behaviour was assessed by the occurrence of pain or discomfort during the previous 12 months, frequency and reasons for dental check-ups, as well as the frequency, practices and aids of oral hygiene [25].
To gain a deeper understanding of the factors that contribute to oral health, a scientific approach was employed to examine the associations between specific characteristics of children (such as gender, age, and parental education) and their oral health. Furthermore, the study investigated the connection between dietary behaviours and three clinical indices in order to identify any significant variances among Romanian schoolchildren. The clinical indices used were as follows: MT (missing teeth), which represents the number of teeth that have been extracted due to caries and is indicated by the code 97/98; RT (restoration), which indicates the number of surfaces that have undergone restoration or sealing, with high values possible due to each tooth having 4–5 surfaces; and D3T, which represents the number of surfaces with a caries code greater than 3, indicating the presence of dentinal lesions. The codes range from 0 to 6–7, with codes higher than 3 denoting dentinal lesions (while the remaining codes refer to incipient lesions without enamel damage).
The statistical analysis of the questionnaire data was conducted using Statistical Package for the Social Sciences (SPSS) version 23 for Windows. Spearman rank correlation, a nonparametric test denoted by “rs” or “rho”, was employed to assess the strength of the monotonic relationship between quantitative and ordinal variables, with statistical significance being set at p < 0.05.
Results
The study involved 133 schoolchildren, both boys and girls, between the ages of 11 and 14, with an average age of 12.26 years, as presented in Table 1. The sample yielded a DMFT index value of 2.93 ± 2.70.
As part of the study, participants’ personal characteristics and the education levels of both their mothers and fathers were considered as factors influencing children’s oral health. With regard to the mothers’ educational backgrounds, the sample study revealed that 19 individuals had completed secondary school (8th grade), 38 had graduated from high school (12th grade), and 29 had obtained a university degree. Similarly, in terms of the fathers’ education, 15 individuals had completed secondary school, 25 had graduated from high school, and 24 had obtained a university degree (refer to Table 2).
Parental Education Correlates with Eating Habits
According to the results of the study, there was a strong negative statistical association between father’s education and children’s consumption of sweetened beverages (−0.02 **). As for mother’s education, the results also showed a strong negative relationship with the consumption of sweetened beverages (−0.02 **), as well as a negative relationship with the consumption of sugar-sweetened chewing gum (−0.01 *), milk sweetened with sugar or honey (−0.02 *), sweetened tea (−0.02 *) and cocoa sweetened with sugar or honey (−0.01 *) (Table 3).
Parental Education Linked to Preventive Behaviour
According to the results, a positive and significant relationship (rs = 0.17 *, p < 0.05) was found for the relationship between mother’s education and the frequency of visits to the dentist reported by children, which means that the higher the mother’s education level, the higher the number of visits made by the children to the dentist. The relationship between mother’s education and frequency of tooth brushing in children was also positive (rs = 0.02 *, p < 0.05), so the higher the mother’s education, the higher the frequency of tooth brushing in children. Regarding the relationship between father’s education and preventive behaviour, no significant associations were found (Table 5).
Discussion
Limited oral epidemiological studies have been conducted in Romania recently, resulting in a scarcity of systematic data regarding the oral health behaviour of schoolchildren. Existing studies have been confined to small samples within specific regions of the country. This research paper aims to address this gap by examining the impact of parental education on the preventive habits and oral health status of 11–14-year-old students residing in urban and rural areas of western Romania. The data gathered in this study were statistically representative of the western region. Given the significance of oral health issues among schoolchildren, identifying influential factors that contribute to the prevalence of caries is crucial for effective preventive measures.
Data from the literature show that low levels of parental education are linked to high caries risk among schoolchildren. The level of education among parents influences their perspectives on their children’s oral health. According to a study conducted by Rajab et al., it was found that parents with higher education levels displayed greater concern for their children’s oral health [29]. Inadequate parental education is recognised as a key contributor to subpar oral health among children. Furthermore, research has consistently linked parental education levels to the socioeconomic status of the family [30]. According to findings from Italy, it was observed that children whose parents had a higher level of education had a lower incidence of cavities compared to children whose parents had a lower level of education [28]. Children from families with highly educated parents were more likely to benefit from restorative treatment [27]. Data from the literature have shown that low parental educational attainment has been linked to high caries risk among schoolchildren [31]. There appears to be a tentative correlation between a limited level of maternal education and an increased incidence of dental caries [32]. The greater the educational attainment of parents, the more positively their children engage in oral self-care [16]. The findings indicate a clear association between socioeconomic factors and the occurrence of dental caries. Consequently, it is imperative to implement extensive educational interventions targeting parents with limited education. Various countries have already initiated effective oral health promotion programmes to combat the disease and enhance the oral well-being of school-aged children. It is crucial to integrate children’s oral health programmes with other public health sectors for a comprehensive approach to improve overall public health [18]. Fluoride is emerging as a highly effective and minimally intrusive solution for combating dental diseases, with dental caries being a prime concern. Incorporating fluoride into public health interventions has shown promising results in reducing the prevalence of dental caries. The fluoridation of water and the use of fluoride toothpaste, gel, and mouthwash are among the commonly employed preventive measures to manage dental caries [33]. In recent studies, it has been shown that the oral health of children has experienced notable enhancements as a result of various preventive measures. These include the implementation of fluoride, toothpaste usage, dental sealant treatments, and community water fluoridation programmes. The literature provides compelling evidence that these approaches have played a significant role in the overall improvement of children’s oral health [34].
One of the study’s limitations is the potential bias in interpreting the results, stemming from the study design itself. Cross-sectional studies, which measure cause and effect simultaneously, introduce temporal ambiguity and hinder the establishment of causal relationships. Furthermore, it is crucial to acknowledge that the questionnaire’s data source may not be entirely reliable, particularly regarding socio-economic information.
The validity of the findings is bolstered by the rigorous sample selection and data analysis processes, as well as the meticulous calibration process. This study not only examines the prevalence of caries, but also evaluates the impact of significant caries risk factors and oral health behaviours using the STEPS model, as recommended by WHO guidelines [35]. This approach enables the assessment and comparison of national trends with those in other countries. The STEPS approach emphasises the importance of regular and continuous data collection.
Conclusions
In summary, the findings indicate a significant link between the oral health condition, preventive habits, and the educational background of parents/caregivers of children residing in the western region of Romania. The outcomes imply that a higher occurrence of tooth decay may be associated with limited educational attainment among parents. The study extensively elucidates the oral health status of children aged 11–14 years in the western region of Romania, serving as foundational information for future investigations and showcasing the socio-economic influence on dental caries prevalence. The gathered data can subsequently be utilised to formulate and execute sustainable oral–dental prevention programmes aimed at enhancing the oral health of schoolchildren.
Author Contributions
Conceptualisation, R.D., R.S.-R.; Methodology, R.S.-R.; Software, D.N.; Validation. D.N. and R.S.-R.; Formal Analysis, O.B.; Investigation, R.D. I.G.P.; Resources, D.J.; Data Curation, A.G.; Writing—Original Draft Preparation, O.B.; Writing—Review and Editing, R.D.; Visualisation, R.O.; Supervision, A.G.; Project Administration, O.B.; Funding Acquisition, R.S.-R.
Acknowledgments
The authors are grateful to the schoolteachers and school workers for the help that they provided in this survey. A special thanks goes to the children and parents who participated in the survey. Collaborators on the Oral Health Survey for Children in Romania are: Ruxandra Sfeatcu (Oral Health and Community Dentistry Department, Faculty of Dental Medicine, UMP “Carol Davila”, Bucharest), Mariana Caramida (Oral Health and Community Dentistry Department, Faculty of Dental Medicine, UMP “Carol Davila”, Bucharest), Anca Stefania Mesaros (Department of Dental Propaedeutic, “Iuliu Hatieganu” University of Medicine and Pharmacy Cluj-Napoca, Romania), Alexandru Mester (Department of Oral Health, “Iuliu Hatieganu” University of Medicine and Pharmacy, Cluj-Napoca, Romania), Ioana Constantin (Department of Pedodontics, County Hospital Cluj-Napoca, Cluj Napoca, Romania), Nora Orban (Department of Pedodontics, County Hospital Cluj-Napoca, Cluj Napoca, Romania), Lavinia Cosma (Department of Pedodontics, “Iuliu Hatieganu University of Medicine and Pharmacy, Cluj-Napoca, Romania), Sebastian Candrea (Department of Pedodontics, County Hospital Cluj-Napoca, Romania), Luminita Dăguci (Department of Preventive and Oral Health, Faculty of Dentistry, University of Medicine and Pharmacy, Craiova, Romania), Marilena Bataiosu (Department of Pedodontics, Faculty of Dentistry, University of Medicine and Pharmacy, Craiova, Romania), Carina Balcos (“Grigore T. Popa” University of Medicine and Pharmacy Iasi, Faculty of Dental Medicine, Department of Oro-Dental Prevention, Iasi, Romania) and Lucia Magda Barlean (“Grigore T. Popa” University of Medicine and Pharmacy Iasi, Faculty of Dental Medicine, Department of Oro-Dental Prevention, Iasi, Romania).
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Kassebaum, N.J.; Smith, A.G.C.; Bernabé, E.; Fleming, T.D.; Reynolds, A.E.; Vos, T.; Murray, C.J.L.; Marcenes, W.; GBD 2015 Oral Health Collaborators; Abyu, G.Y.; et al. Global, Regional, and National Prevalence, Incidence, and Disability-Adjusted Life Years for Oral Conditions for 195 Countries, 1990–2015: A Systematic Analysis for the Global Burden of Diseases, Injuries, and Risk Factors. J. Dent. Res. 2017, 96, 380–387. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Ending Childhood Dental Caries: WHO Implementation Manual; World Health Organization: Geneva, Switzerland, 2019; ISBN 978-92-4-000005-6. [Google Scholar]
- Chaffee, B.W.; Rodrigues, P.H.; Kramer, P.F.; Vítolo, M.R.; Feldens, C.A. Oral Health-Related Quality-of-Life Scores Differ by Socioeconomic Status and Caries Experience. Community Dent. Oral Epidemiol. 2017, 45, 216–224. [Google Scholar] [CrossRef]
- Park, K. Park’s Textbook of Preventive and Social Medicine, Twenty-third edition; Bhanot Publishers: Bhopal, India, 2015; ISBN 978-93-82219-05-7. [Google Scholar]
- Glick, M.; Williams, D.M.; Kleinman, D.V.; Vujicic, M.; Watt, R.G.; Weyant, R.J. A New Definition for Oral Health Developed by the FDI World Dental Federation Opens the Door to a Universal Definition of Oral Health. J. Am. Dent. Assoc. 2016, 147, 915–917. [Google Scholar] [CrossRef] [PubMed]
- Watt, R.G.; Mathur, M.R.; Aida, J.; Bönecker, M.; Venturelli, R.; Gansky, S.A. Oral Health Disparities in Children. Pediatr. Clin. N. Am. 2018, 65, 965–979. [Google Scholar] [CrossRef]
- Watt, R.G.; Sheiham, A. Integrating the Common Risk Factor Approach into a Social Determinants Framework. Community Dent. Oral Epidemiol. 2012, 40, 289–296. [Google Scholar] [CrossRef]
- Petersen, P.E.; Bourgeois, D.; Ogawa, H.; Estupinan-Day, S.; Ndiaye, C. The Global Burden of Oral Diseases and Risks to Oral Health. Bull. World Health Organ. 2005, 83, 661–669. [Google Scholar]
- Edelstein, B.L.; Chinn, C.H. Update on Disparities in Oral Health and Access to Dental Care for America’s Children. Acad. Pediatr. 2009, 9, 415–419. [Google Scholar] [CrossRef] [PubMed]
- Do, L.G.; Spencer, A.J.; Slade, G.D.; Ha, D.H.; Roberts-Thomson, K.F.; Liu, P. Trend of Income-Related Inequality of Child Oral Health in Australia. J. Dent. Res. 2010, 89, 959–964. [Google Scholar] [CrossRef]
- Dye, B.A.; Arevalo, O.; Vargas, C.M. Trends in Paediatric Dental Caries by Poverty Status in the United States, 1988-1994 and 1999–2004. Int. J. Paediatr. Dent. 2010, 20, 132–143. [Google Scholar] [CrossRef] [PubMed]
- Bernabeé, E.; Hobdell, M.H. Is Income Inequality Related to Childhood Dental Caries in Rich Countries? J. Am. Dent. Assoc. 2010, 141, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Fisher-Owens, S.A.; Gansky, S.A.; Platt, L.J.; Weintraub, J.A.; Soobader, M.-J.; Bramlett, M.D.; Newacheck, P.W. Influences on Children’s Oral Health: A Conceptual Model. Pediatrics 2007, 120, e510–e520. [Google Scholar] [CrossRef]
- Adair, P.M.; Pine, C.M.; Burnside, G.; Nicoll, A.D.; Gillett, A.; Anwar, S.; Broukal, Z.; Chestnutt, I.G.; Declerck, D.; Ping, F.X.; et al. Familial and Cultural Perceptions and Beliefs of Oral Hygiene and Dietary Practices among Ethnically and Socio-Economicall Diverse Groups. Community Dent. Health 2004, 21, 102–111. [Google Scholar]
- Efe, E.; Sarvan, S.; Kukulu, K. Self-Reported Knowledge and Behaviors Related to Oral and Dental Health in Turkish Children. Issues Compr. Pediatr. Nurs. 2007, 30, 133–146. [Google Scholar] [CrossRef] [PubMed]
- Castilho, A.R.F.d.; Mialhe, F.L.; Barbosa, T.d.S.; Puppin-Rontani, R.M. Influence of Family Environment on Children’s Oral Health: A Systematic Review. J. Pediatr. 2013, 89, 116–123. [Google Scholar] [CrossRef]
- Peres, M.A.; Barros, A.J.; Peres, K.G.; Araújo, C.L.P.; Menezes, A.M.B. Life Course Dental Caries Determinants and Predictors in Children Aged 12 Years: A Population-Based Birth Cohort. Community Dent. Oral Epidemiol. 2009, 37, 123–133. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.J.; Gao, S.S.; Duangthip, D.; Lo, E.C.M.; Chu, C.H. Early Childhood Caries and Oral Health Care of Hong Kong Preschool Children. CCIDE 2019, 11, 27–35. [Google Scholar] [CrossRef]
- Mueller, M.; Schorle, S.; Vach, K.; Hartmann, A.; Zeeck, A.; Schlueter, N. Relationship between Dental Experiences, Oral Hygiene Education and Self-Reported Oral Hygiene Behaviour. PLoS ONE 2022, 17, e0264306. [Google Scholar] [CrossRef]
- Chen, L.; Hong, J.; Xiong, D.; Zhang, L.; Li, Y.; Huang, S.; Hua, F. Are Parents’ Education Levels Associated with Either Their Oral Health Knowledge or Their Children’s Oral Health Behaviors? A Survey of 8446 Families in Wuhan. BMC Oral Health 2020, 20, 203. [Google Scholar] [CrossRef]
- Saldūnaitė, K.; Bendoraitienė, E.A.; Slabšinskienė, E.; Vasiliauskienė, I.; Andruškevičienė, V.; Zūbienė, J. The Role of Parental Education and Socioeconomic Status in Dental Caries Prevention among Lithuanian Children. Medicina 2014, 50, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Petersen, P.E. The World Oral Health Report 2003: Continuous Improvement of Oral Health in the 21st Century—the Approach of the WHO Global Oral Health Programme: The World Oral Health Report 2003. Community Dent. Oral Epidemiol. 2003, 31, 3–24. [Google Scholar] [CrossRef]
- Rowan-Legg, A. Oral Health Care for Children—A Call for Action. Paediatr. Child Health 2013, 18, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Sheiham, A. Dental Caries Affects Body Weight, Growth and Quality of Life in Pre-School Children. Br. Dent. J. 2006, 201, 625–626. [Google Scholar] [CrossRef] [PubMed]
- Dumitrescu, R.; Sava-Rosianu, R.; Jumanca, D.; Balean, O.; Damian, L.-R.; Fratila, A.D.; Maricutoiu, L.; Hajdu, A.I.; Focht, R.; Dumitrache, M.A.; et al. The Impact of Parental Education on Schoolchildren’s Oral Health—A Multicenter Cross-Sectional Study in Romania. Int. J. Environ. Res. Public Health 2022, 19, 11102. [Google Scholar] [CrossRef]
- Sava-Rosianu, R.; Campus, G.; Matichescu, A.; Balean, O.; Dumitrache, M.A.; Lucaciu, P.O.; Daguci, L.; Barlean, M.C.; Maricutoiu, L.; Postolache, M.; et al. Caries Prevalence Associated with Oral Health-Related Behaviors among Romanian Schoolchildren. Int. J. Environ. Res. Public Health 2021, 18, 6515. [Google Scholar] [CrossRef]
- Dumitrescu, R.; Sava-Rosianu, R.; Jumanca, D.; Balean, O.; Damian, L.-R.; Campus, G.G.; Maricutoiu, L.; Alexa, V.T.; Sfeatcu, R.; Daguci, C.; et al. Dental Caries, Oral Health Behavior, and Living Conditions in 6–8-Year-Old Romanian School Children. Children 2022, 9, 903. [Google Scholar] [CrossRef] [PubMed]
- Lamster, I.B. The 2021 WHO Resolution on Oral Health. Int. Dent. J. 2021, 71, 279–280. [Google Scholar] [CrossRef]
- Rajab, L.D.; Petersen, P.E.; Bakaeen, G.; Hamdan, M.A. Oral Health Behaviour of Schoolchildren and Parents in Jordan: Oral Health Behaviour in Jordan. Int. J. Paediatr. Dent. 2002, 12, 168–176. [Google Scholar] [CrossRef]
- Pizzo, G.; Piscopo, M.R.; Matranga, D.; Luparello, M.; Pizzo, I.; Giuliana, G. Prevalence and Socio-Behavioral Determinants of Dental Caries in Sicilian Schoolchildren. Med. Sci. Monit. 2010, 16, PH83–89. [Google Scholar]
- Gorgi, Z.; Abbasi, A.; Mohsenzadeh, A.; Damankeshan, A.; Sheikh Fathollahi, M. A Survey on DMFT Index of the First Permanent Molar in 12-Year-Old Students of Larestan, Iran, in 2014. J. Occup. Health Epidemiol. 2017, 6, 32–39. [Google Scholar] [CrossRef]
- Peres, M.A.; Macpherson, L.M.D.; Weyant, R.J.; Daly, B.; Venturelli, R.; Mathur, M.R.; Listl, S.; Celeste, R.K.; Guarnizo-Herreño, C.C.; Kearns, C.; et al. Oral Diseases: A Global Public Health Challenge. Lancet 2019, 394, 249–260. [Google Scholar] [CrossRef] [PubMed]
- Muñoz-Millán, P.; Zaror, C.; Espinoza-Espinoza, G.; Vergara-Gonzalez, C.; Muñoz, S.; Atala-Acevedo, C.; Martínez-Zapata, M.J. Effectiveness of Fluoride Varnish in Preventing Early Childhood Caries in Rural Areas without Access to Fluoridated Drinking Water: A Randomized Control Trial. Community Dent. Oral Epidemiol. 2018, 46, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Petersen, P.E.; Lennon, M.A. Effective Use of Fluorides for the Prevention of Dental Caries in the 21st Century: The WHO Approach. Commun. Dent. Oral Epidemiol. 2004, 32, 319–321. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.who.int/publications/who-guidelines (accessed on 28.05.2023).
Figure 1.
Schematic of the workflow in the sampling stage.
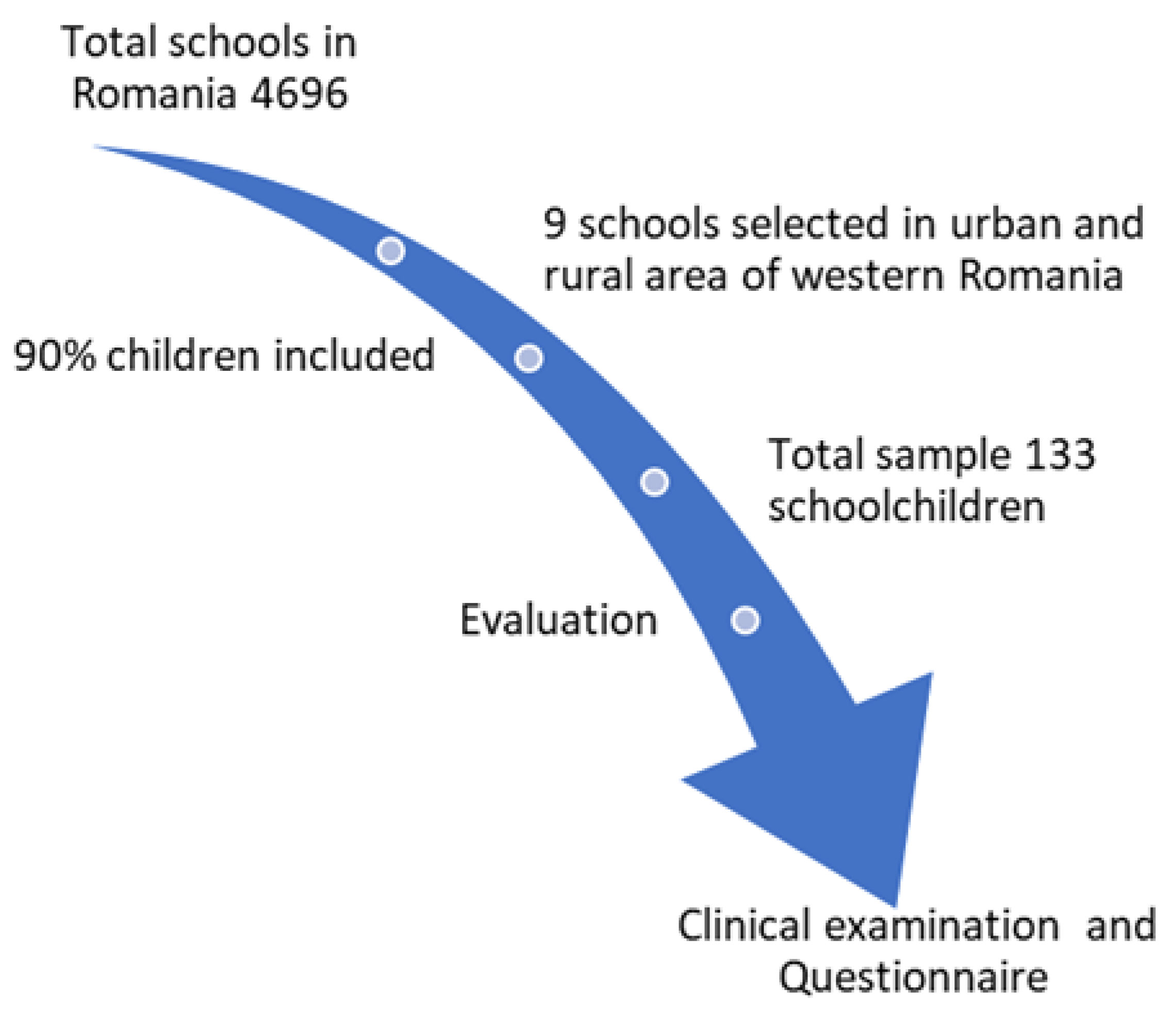
Table 1.
Gender and age description of the sample.
| Variable | N (%) | |
|---|---|---|
| Gender | Boys | 72 (54.1) |
| Girls | 61 (45.9) | |
| Age | 11 years | 4 (3%) |
| 12 years | 94 (70.7%) | |
| 13 years | 32 (24.1%) | |
| 14 years | 3 (2.3%) | |
Table 2.
Description of the sample according to mother’s and father’s education.
| Level of Education | Mothers’ Education (%) | Fathers’ Education (%) |
|---|---|---|
| No school | 1 (0.73) | 1 (0.49) |
| Primary school (grade 0–4) | 3 (2.44) | 4 (2.93) |
| Gymnasium (grade 0–8) | 19 (14.90) | 15 (11.11) |
| Professional school (grade 0–10) | 18 (13.80) | 20 (15.14) |
| High school (grade 0–12) | 38 (28.57) | 25 (32.72) |
| Professional School | 7 (5.37) | 5 (3.54) |
| University degree | 29 (22.10) | 24 (18.19) |
| I don’t know/I don’t answer | 14 (10.62) | 17 (12.94) |
| I don’t leave with a mother figure/father figure in the house | 1 (0.37) | 2 (1.95) |
Table 3.
Correlation between eating behaviour and parental education (* p < 0.05, ** p < 0.01).
| Eating Habits | Father’s Education rs-rho(p,N) | Mother’s Education rs-rho(p,N) |
|---|---|---|
| Fresh fruit | −0.01 (0.01, 133) | −0.08 (0.03, 133) |
| Biscuits, cakes, creams, sweets, pies, sweets | 0.03 (0.06, 133) | −0.08 (0.03, 133) |
| Sweetened drinks | −0.02 ** (0.00, 133) | −0.02 ** (0.00, 133) |
| Jam/honey | −0.01 (0.08, 133) | −0.00 (0.09, 133) |
| Chewing gum with sugar | −0.02 (0.07, 133) | −0.01 * (0.02, 133) |
| Sweets/candies | −0.04 (0.05, 133) | −0.01 (0.00, 133) |
| Milk sweetened with sugar/honey | −0.01 (0.02, 133) | −0.02 * (0.00, 133) |
| Sweetened tea | −0.07 (0.03, 133) | −0.02 * (0.00, 133) |
| Cocoa sweetened with sugar/honey | −0.05 (0.03, 133) | −0.01 * (0.00, 133) |
Table 4.
Correlation between parental education and clinical status (* p < 0.05, ** p < 0.01).
| Type of Index | Mother’s Education rs-rho(p,N) | Father’s Education rs-rho (p,N) |
|---|---|---|
| MT | −0.01 (0.10, 133) | 0.04 (0.59, 133) |
| D3T | −0.26 ** (0.02, 133) | −0.17 * (0.04, 133) |
| RT | 0.15 (0.08, 133) | 0.01 (0.08, 133) |
| DMFT | −0.15 (0.06, 133) | −0.16 (0.05, 133) |
Table 5.
Correlation between parental education and type of preventive behaviour (* p < 0.05, ** p < 0.01).
Table 5.
Correlation between parental education and type of preventive behaviour (* p < 0.05, ** p < 0.01).
| Type of Preventive Behaviour | Mother’s Education rs-rho (p, N) | Father’s Education rs-rho (p, N) |
|---|---|---|
| Tooth pain in the last 12 months | −0.15 (0.07, 133) | −0.11 (0.17, 133) |
| Frequency of hygiene methods (toothbrushing) | 0.02 * (0.02, 133) | 0.15 (0.08, 133) |
| Frequency of visits to the dentist in the last 12 months | 0.17 * (0.04, 133) | 0.01 (0.21, 133) |
© 2023 Copyright by the authors. Licensed as an open access article using a CC BY 4.0 license.


